Independent Study Highlights Big Gains for AI-Assisted Primary Care
A new study from Phyx Primary Care’s Innovation Lab found that an AI copilot can significantly ease the transition to value-based care for primary care practices. The lab’s independent evaluation examined Navina’s AI copilot, a clinical assistant that integrates into existing electronic health records (EHRs) solutions. The findings point to measurable improvements in physician burnout, documentation efficiency, and key value-based care metrics after the AI tool was deployed across 19 primary care practices. Participating physicians reported spending less time on onerous paperwork and more time on patient care, all while achieving better risk scores and quality ratings.
For clinics accustomed to fee-for-service, value-based care (or VBC) represents a wholesale shift from counting visits to measuring outcomes. The operational lift is steep. Most primary-care groups face an expanding set of value-based obligations such as precise risk adjustment, quality reporting, and real-time utilization management. Today, many groups straddle both fee-for-service and value-based models, creating what the report called “a foot in two canoes” – an administrative balancing act that heightens burnout risk and leaves little bandwidth for patient care.
Navina helps face this challenge by deploying powerful AI to synthesize fragmented patient data–labs, consult notes, prior visits, and more into actionable, problem-oriented summaries that support clinical decision-making, documentation and coding at the point of care. Instead of clicking through dozens of tabs, the physician sees one integrated view of the patient’s history, active issues, and care opportunities. Navina flags potential diagnoses, highlights care gaps, such as chronic conditions missing proper documentation, and suggests appropriate risk adjustment codes and quality actions in real-time. Each actionable insight is linked to the original clinical evidence.
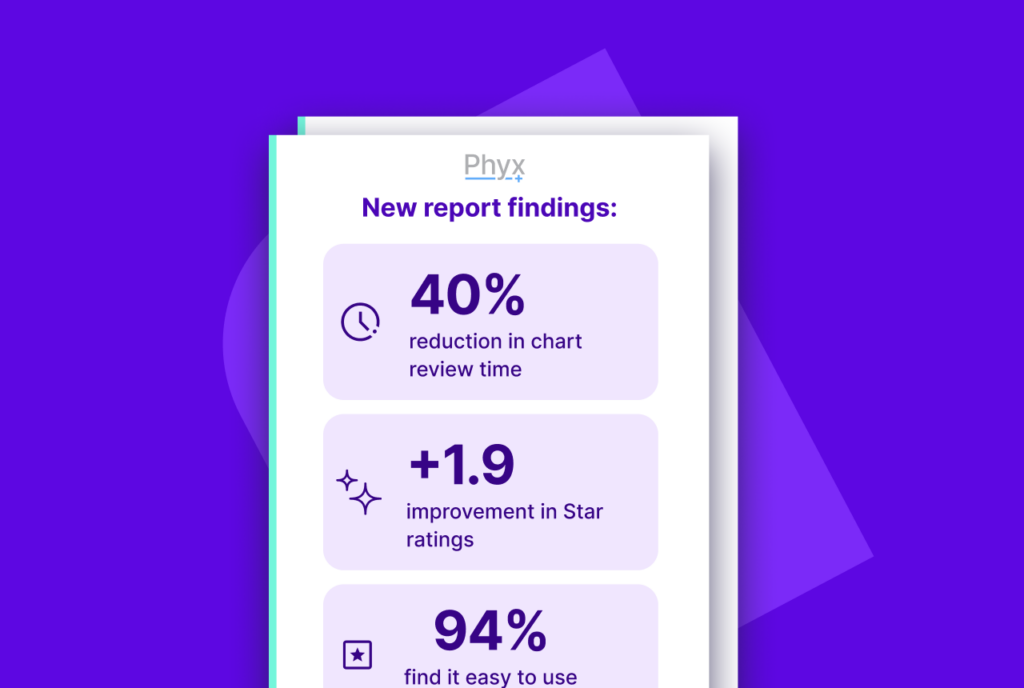
One of the most striking outcomes in the study is the reduction in administrative workload. A survey of 120 primary care physicians who used Navina’s AI copilot for at least 30 days found that the average chart review time for complex visits dropped by 40%. Doctors also reported that their chart review burden fell by 24%, while the share of appointments they entered feeling fully prepared rose by 12%.
These gains translated into tangible relief for doctors. Using their Primary Care Vital Signs® framework, Phyx’s researchers found a 32% reduction in physician burnout among the cohort, accompanied by a 23% decline in reported dissatisfaction with their work. 84% of the physicians said they would recommend Navina to a colleague – a strong vote of confidence in the solution’s value.
Physicians surveyed described the impact in their own words. “The Assistant finds new diagnoses buried in the record — things I’d miss. That can be the difference between staying afloat or falling behind,” said one physician. “It gives me hope that we can make value-based care work,” said another.
Navina’s AI copilot went beyond improving physicians’ professional wellbeing, to improve performance metrics that directly affect the bottom line and quality ratings of every value-based healthcare organization. Navina prompts physicians with evidence-based diagnosis and HCC recommendations. According to the report, with Navina, “visit documentation is completed before the patient leaves the exam room.” At the end of the visit, the doctor can feel confident that their chart is “accurate, compliant, and reflects the full clinical picture – essential for VBC performance.”
The data back up these qualitative improvements. 91% of Navina’s HCC recommendations were addressed by physicians during visits, and 73% of those suggestions were ultimately accepted into the documentation. This more thorough capture of patient complexity led to a measurable rise in risk scores. On average, the practices saw their Risk Adjustment Factor (RAF), a key value-based payment metric, increase by +0.153, indicating improved documentation of illness burden. Quality metrics saw a boost as well: clinics reported an average +1.9 point gain in their Star quality ratings across 32 measures, from preventive screenings to chronic disease management. These improvements translate directly into higher shared savings and performance incentives under value-based contracts.
Crucially, physicians trusted Navina’s AI, with 92% reporting they trusted the assistant’s HCC coding suggestions, and 85% trusting its diagnostic prompts. Notably, 94% of physicians found the tool easy to use and access during their workflow – a testament to the importance of seamless integration with existing clinical workflows. High adoption followed: 90% of physicians were using Navina’s AI copilot at least weekly by the end of the trial. In short, the solution gained both trust and ‘stickiness’ with frontline users, boding well for sustained improvements.
For healthcare leaders and primary care physicians alike, an AI assistant tailored for VBC is no longer a futuristic nice-to-have, but a practical necessity. For physicians struggling under mounting paperwork and performance targets, tools like Navina’s may offer a lifeline, improving care quality and financial outcomes while letting physicians focus on what matters most: the patient in front of them.
Read the full Phyx Innovation Lab report here.